This year marks the 10th anniversary of the Institute for Better Health (IBH)!
Founded in 2014 by a team of change makers at Trillium Health Partners (THP), IBH was created with a simple but powerful pursuit: to create better health for patients, families and our community. From the beginning, we have done this through the application of best-in-class research and innovation to the address the problems our health system and its patients are facing each day. At IBH, we are continually driven by a passion to care for others, push the boundaries of traditional research and innovation, and make meaningful, sustainable change in partnership with the communities we serve.
Our 2023-24 Annual Report captures how we achieve our ambitions and highlights the amazing teams, partners and community members who inspire us to approach research and innovation differently. In the stories that follow, we share on-the-ground examples of how our work is truly helping to create a new kind of health care for a healthier community.
Over the past decade and into today, IBH has grown to lead Learning Health Systems and population health science, innovation and thought leadership across Canada. As a result, THP was recognized as one of Canada’s Top 40 Research Hospitals by Research Infosource Inc. for a second consecutive year. IBH is at the helm of this achievement - boldly advocating, innovating and applying our expertise to ensure our diverse and growing community receives high-quality, accessible and sustainable health care.
With an aging population and workforce, greater health complexities, widening inequities and persistent capacity challenges, the need to mobilize knowledge into practice has never been more important. Together with our community, we’re co-designing a system that works for everyone and can be replicated in other communities within Canada and worldwide.
This year, the framework describing the way we work and create change was published in the seminal Learning Health Systems Action Framework. It was built and refined at IBH in collaboration with the Ontario Strategy for Patient-Oriented Research Support Unit (OSSU), health system leaders, researchers, patients and community members. This important milestone is the culmination of learning and collaboration across all parts of our health system to truly understand what is required to co-design, implement and sustain change in pursuit of better health. The framework is now being used across the country to help other health systems meaningfully move from evidence to action to impact. Our Annual Report brings to life how the Learning Health System is actioned each and every day at THP through meaningful collaboration between our scientists, researchers, innovators and frontline staff.
We’ve also grown our innovation capabilities, deepening our commitment to improving the health of our community by creatively addressing the day-to-day challenges THP faces head-on in partnership with frontline staff, care providers, patients, families and community members. We will be profiling innovation in-depth through a dedicated report later this year.
Our accomplishments over this past year would not be possible without the continued support of the IBH team and our hospital. Most importantly, we thank our patients, families and community members for your support in creating a healthier, more inclusive tomorrow.
Thank you,
Dr. Rob Reid,
Hazel McCallion Research Chair in Learning Health Systems, Institute for Better Health, and Senior Vice President, Science, Trillium Health Partners
Simone Harrington,
Vice President, Institute for Better Health
Driving the Learning Health System Forward
The Learning Health System (LHS) – rapid cycle research and innovation embedded in health systems to improve patient care in real-time – has been implemented and scaled with increased momentum at Trillium Health Partners (THP) and beyond, demonstrating the Institute for Better Health’s (IBH) leadership in driving LHS research and innovation forward to advance health equity and population health for a healthier tomorrow.
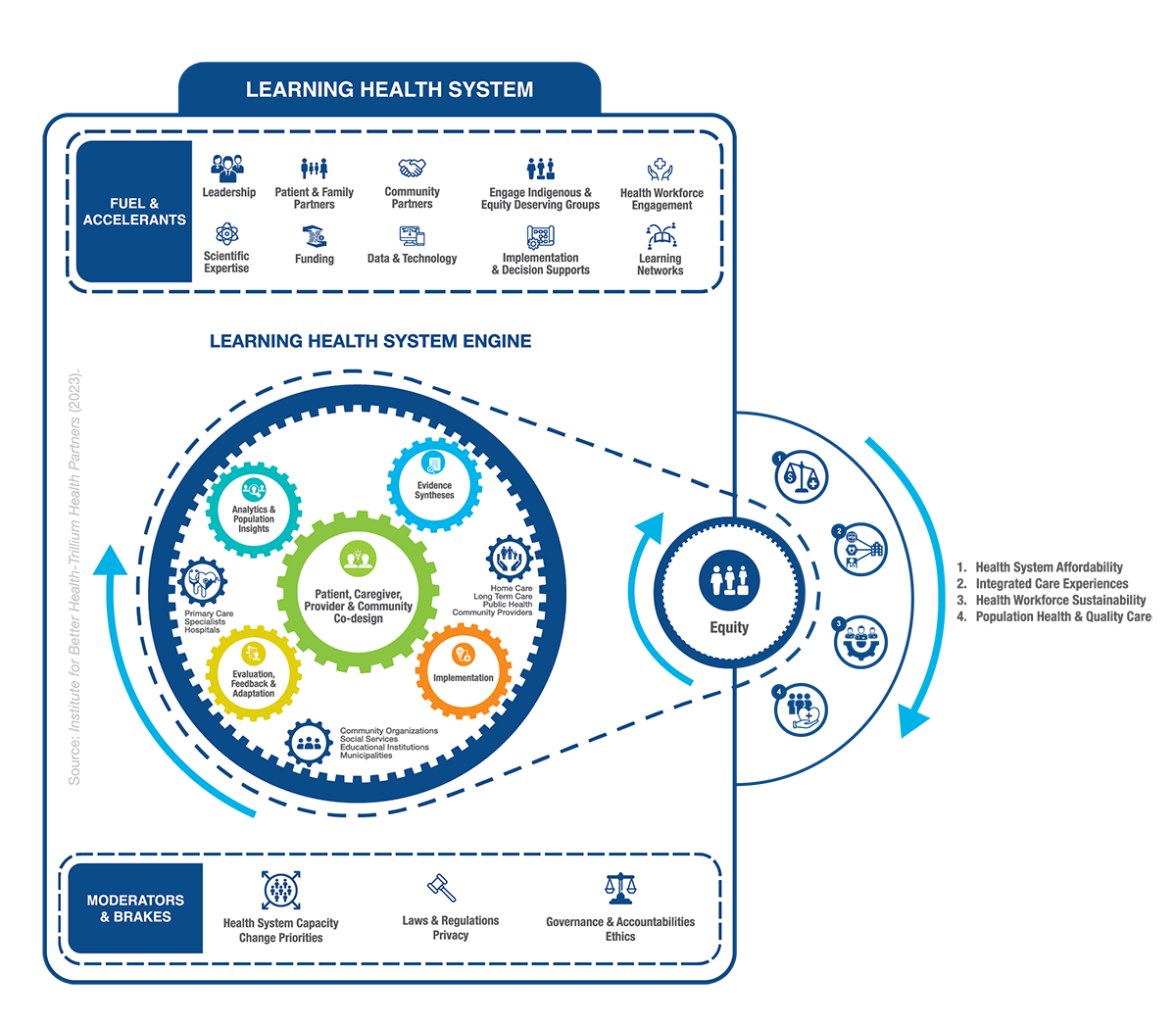
This year, IBH launched the Learning Health System Action Framework, which describes how research and health care operations are linked and enacted in a comprehensive LHS approach to advance population health and health equity.
The Framework, built and refined by IBH Scientists in collaboration with the Ontario Strategy for Patient-Oriented Research Support Unit (OSSU), was launched at OSSU’s 2023 Research Day and published in SSM – Health Systems. Health systems and researchers who seek to implement an LHS approach are using this framework to identify capabilities necessary to systematically enact the learning elements.
LHS Accelerator Grants
IBH created our LHS Accelerator Grants two years ago to fund Learning Health Systems-focused research on the frontlines of care at THP. The LHS Accelerator Grants engaged multidisciplinary teams of scientists, research associates, students, and THP operational leaders to advance innovative and impactful research that helps respond to key challenges needed to improve the health of the Peel population.
In response to the strength of the submissions and in the spirit of the impact for which this award is intended, the funding envelope was increased from $75,000 to $150,000 with philanthropic support from the THP Foundation and awarded across seven key projects. “The goal for this funding program is to catalyze new, emerging and early-stage research ideas that will provide the insights needed for larger co-design efforts, evaluations and trials while also building Learning Health System capacity at THP,” says Dr. Laura Desveaux, Scientific Director and Learning Health System Lead, IBH. “The partnerships across the applications are a testament to the growth in both our LHS capabilities and our collaborative relationships in the pursuit of improving population health and shaping a healthier tomorrow.”
Hazel McCallion Annual Lecture in Shaping Healthier Communities


IBH hosted its fourth Hazel McCallion Annual Lecture in Shaping Healthier Communities titled “Advancing the Learning Health System: Insights from Beyond Health Care” at Sheridan College’s Hazel McCallion Campus on December 5, 2023. The keynote presentation was delivered by renowned thought leaders Dr. Rob Reid, Hazel McCallion Research Chair in Learning Health Systems, IBH, and Keddone Dias, Executive Director, LAMP Community Health Centre, who envisioned what a new kind of health care for a healthier community looks like, and how to get there using the LHS framework at the hospital and the community level, emphasizing the importance of integrating and centering diverse patient, family and community voices.
Panelists Amie Archibald-Varley, Registered Nurse, Women’s Health CEO, Advancing Health Equity, Together, CBC Freelance Journalist, author of The Wisdom of Nurses (Harper Collins, 2024), and Dr. Hayley Wickenheiser, four-time Olympic Gold Medalist, Physician and Assistant General Manager of Player Development for the Toronto Maple Leafs, joined IBH Scientific Director and LHS Program Lead, Dr. Laura Desveaux, as well as Dr. Reid and Dias for an interactive panel discussion following the presentation. The panel focused on how to drive transformational change in the health-care system with a focus on equity as a key outcome.
Award-Winning LHS Research
Recent funding from the Canadian Institutes of Health Research (CIHR) is being allocated in support of building LHS capacity across THP and our community. Through a CIHR Health Systems Impact Early Career Researcher Award, Dr. Marissa Bird, LHS Scientist, will be examining the concept of Organizational Ambidexterity and its potential to increase health system capacity to meet the needs of a growing and aging population.
The concept of Organizational Ambidexterity allows organizations to balance their innovation efforts with sustaining existing pockets of excellence so that we can create better health together in an evidence-based way. "Understanding this paradox is central to building leadership capacity in health systems today, which requires that individuals and teams think, work, and partner differently – with each other and with the communities we serve – to meet the increasingly complex, volatile and unpredictable world," says Dr. Bird. The work supports building internal capacity for sustainable innovation at THP by identifying what ambidextrous capabilities look like in practice and the context(s) in which they lead to better outcomes.
Innovating on the Frontlines
Innovation champions the ideas originating from the direct experiences of those intimately involved with the health system: patients, families, caregivers and care providers. The Institute for Better Health (IBH) will support and cultivate these solutions directly within the care setting and in the community through fundamental innovations aimed at enhancing the way we work and deliver care, ultimately contributing to better health for our community.
Read on for this year’s innovation highlights.
Digitizing the Supply Catalogue at THP

Introducing the Digital Supply Catalogue - the brainchild of David Black, Innovation Analyst, Strategic Design and Business Development (SDBD), IBH, and 2021 Maria Racioppo Scholarship winner. This solution replaces paper binders with a fully digitized inventory application that units can easily see and update (including photos) in real-time and order what’s needed, streamlining processes to better enable departments across the hospital can get the tools, PPE and equipment needed to do their jobs safely and effectively.
The Digital Supply Catalogue was co-designed with IBH’s SDBD team members and has received accolades from THP’s frontline staff for its user-friendliness. “These little pebbles in our shoes - like having to ask the nursing staff for additional information about ordering supplies - add up,” says one clinical manager. “Solutions like this go a long way.”
Following implementation of a six-month pilot, David and team will focus on key performance indicators and report findings to determine next steps, including enhancements or additional functionality.
THP's Change Makers
The Innovation Awards ceremony took place in October 2023, during Patient Safety Week, and highlighted and celebrated the inspiring change makers and innovators across Trillium Health Partners. Spearheaded by IBH, the Innovation Awards are a way to recognize the incredible work being done at THP, to celebrate our colleagues across the hospital and gain a greater understanding of how interprofessional teams are working together to help shape the future of health care.
Let’s look at this year’s winners:

Service Innovation
“A NATural Solution: Developing a Family Medicine Inpatient Newborn Assessment Team in a Community Academic Hospital” by Dr. Sapna Khosla, Dr. Jane Healey, Dr. Ali Damji, Candace Davidson, Dr. Ian Zenlea, Dr. Catherine Taylor, Joanna Wager, Dr. Hannah Wigle and Karen Hunter

Access Innovation
“THP-OSP Renal Mental Health Initiative” by Andres Gomez, Philip Boll, Devi Ahuja, Brittany Britton, Kylie Katz, Gloria Mullin, Anitaa Gregory and Helen Diasnes-Baluca

Sustainable Innovation
“Integrating Internationally Educated Nurses at THP” by Joy Navaroj, Desa Dlugosz, Kate Smith-Eivemark, Sarah Smith and Anika Andal

Trailblazer Innovation
“High Risk Skin Breakdown Patients and Ensuring Air Bed Allocation” by Amrinder Grewal, Shobha Dookran, Samia Matta, Daniela Negrescu and Patricia Naval

Trailblazer Innovation
“Revitalizing the UCA Role in the NICU-Mississauga Hospital Through the Implementation of the UCA Work & Message Sheets” by Zoe Paget, Vidya Mattai, Angela Sherpa, Naila Zafar, Leila Youssefi, Judy Gane, Sophiya Daniel, Maureen O’Hara, Carol Blair-Murdoch, Molly Shoo, Lena Lloyd and Beverly Belbin

2023 Maria Racioppo Scholarship for Integrative Care
Darwin Ayala, Clinical Clerical Assistant, NeuroMSK, is the recipient of the 2023 Maria Racioppo Scholarship for Integrative Care. This annual Scholarship provides an opportunity for a THP staff member to have dedicated research and innovation time to work on projects and be mentored by IBH team members.
Connecting With Our Community
At the Institute for Better Health (IBH), we champion meaningful collaboration with patients, families, community members and organizations to break down barriers and co-design health services and supports that deeply resonate with the needs and preferences of those we serve.
We know that patient, caregiver and community (PCC) engagement is a key ingredient in Learning Health Systems (LHS) to improve health care service delivery and ultimately health outcomes. “Positioning Patients to Partner,” a commentary led by Dr. Nakia Lee-Foon, Health Equity Research Lead, IBH, found that while many systems are working to include PCCs in helping to improve health care services, for the most part, involvement is limited, incomplete or missed altogether. As the LHS continues gains more traction across health systems, ensuring patients, communities and caregivers are engaged at the onset of research and innovation initiatives and are active and ongoing partners is vital to enhancing health care that is responsive to the people it serves.
Case in point, this year, IBH led transformational work in support of capturing data to better understand and act on patient experience at Trillium Health Partners (THP). Figuring out how to better collect and act on patient data is an issue that hospitals are struggling with globally, and through a LHS approach, informed by the lived experiences of our patients and their families, and in partnership with researchers, program planners, leaders and care providers, THP is testing a digital patient experience survey that could inform implementation in other health contexts across Ontario, Canada and beyond.
Here are the other ways we connected with our community this year, working alongside people and organizations to drive meaningful change and improve health and wellbeing.
Patient, Caregiver and Community Engagement Learning Series
Engaging with patients, caregivers and community members is a critical component of a well-functioning and high-quality health care system. A seven-part online learning series about the core components of patient, caregiver and community engagement was co-designed with patient and caregiver partners, researchers, trainees, health system leaders and providers to meet the learning needs identified by Ontario Health Teams (OHTs). The goal of this learning series was to build connections and competencies for meaningful engagement with patients, caregivers and our community.
The series was led by Dr. Kerry Kuluski, Dr. Mathias Gysler Chair in Patient and Family Centred Care, and the Patient Experience Research Team; it was funded by the Ontario Strategy for Patient-Oriented Research Support Unit (OSSU), with additional in-kind support from the Ministry of Health, Support House’s Centre for Innovation in Peer Support, the Institute for Better Health (Trillium Health Partners), the Ontario Caregiver Organization, and the Rapid Improvement Support and Exchange (RISE) Network.
Reducing Type 2 Diabetes Risk in the Peel Region
People who identify from Black, African and Caribbean (BAC) communities have a higher risk of type 2 diabetes and related complications, and its risk is carried across generations, necessitating a family-based approach to prevention. A Diabetes Canada End Diabetes Award-winning IBH project, “Working Together to Prevent Type 2 Diabetes in Black, African, and Caribbean Communities in Peel, Ontario,” will mobilize community agencies, service providers, researchers and BAC caregivers who have prediabetes, gestational diabetes, or type 2 diabetes or who directly care for a person with type 2 diabetes in co-designing type 2 diabetes prevention interventions that are family-based and culturally sensitive to BAC communities.
Dr. Ian Zenlea, Clinician Scientist and Lead, Family and Child Health Initiative (FCHI), IBH, Paediatric Endocrinologist, THP, and Dr. Dianne Fierheller, Assistant Scientist and Co-Lead, FCHI, will work to centre the voices of the Black, African and Caribbean communities throughout all phases of the project, which will consist of photovoice workshops and a community event. Findings will support ongoing advocacy to co-design more equitable and inclusive interventions for type 2 diabetes prevention that can be tested and adapted to other settings across Canada.


Dr. Terence Tang, a Clinician Scientist at IBH, received a $148,000 Catalyst Grant from the Novo Nordisk Network for Healthy Populations at the University of Toronto for his project aimed at reducing diabetes-related amputations in the region by addressing health inequities. This project will look at the equity-based barriers to receiving foot care that exist for those living with type 2 diabetes in the area, and how to remove those barriers to reduce the number of amputations, a serious diabetes-related complication. Dr. Tang will work with community organizations to look for ways to improve the care pathway and better support those with type 2 diabetes.
Partnering with our Community on Equity-Centred Initiatives
IBH’s Dr. Cilia Mejia-Lancheros, Research Lead of the Family and Child Health Initiative, and Dr. Nakia Lee-Foon, Health Equity Research Lead, are recipients of the inaugural Canadian Institutes of Health Research (CIHR) Research Excellence, Diversity and Independence (REDI) Early Career Transition Awards, which will fund their work in partnering with patients, families and our community to make health services more equitable, inclusive and accessible and to improve health and well-being for everyone. These projects represent two of only 43 prestigious REDI awards distributed to researchers across Canada.
Dr. Mejia-Lancheros’s funded project, “Co-building a community-based and family-focused program to enhance the positive mental well-being of newcomer and refugee families in the Peel Region,” involves co-designing, implementing, and evaluating a community-based, culturally sensitive and family-focused program that aims to improve the positive mental well-being of newcomer families in Peel Region. Together with community-based organizations serving newcomers in Peel, as well as diverse and multidisciplinary supportive teams and peer workforce, including people with lived experiences of immigration with and without mental health challenges, they will co-create mental health and emotional support services for newcomer families settling in Peel and that can be scaled to other settings across Canada.
In Dr. Lee-Foon’s study, “EMPOWHPVR: Exploring the factors that impact HPV-self testing uptake amongst Black women and people with a cervix [WPC] in Peel region, Ontario,” she responds to limited literature on cervical cancer screening amongst Black populations in Canada and an issue observed by community health centres in the Peel region – low cervical cancer screening rates amongst Black WPC. This study will be shaped by Community Research Assistants who identify as Black WPC, community-based organizations that serve Black populations in Peel. Insights collected from patients and service providers (for example, nurses, doctors, social workers) will be used to develop and pilot an intervention that aims to provide Black WPC with information that may empower them to self-sample, which could help detect HPV and precancerous cells earlier, and lead to better outcomes and reduced mortality. This intervention could also help lower health-care costs by reducing clinician-sampled HPV testing and help inform interventions with other equity deserving groups with similar screening rates
Using Population Health Approaches to Shape a Healthier Community
With a relentless commitment to creating a new kind of health care for a healthier community through scientific expertise, innovative thinking and partnerships, the Institute for Better Health (IBH) is a leader in addressing the multifaceted challenges that impact the health and wellbeing of the population.

A cornerstone of the work at IBH focuses on understanding the health of our community and taking a population health-oriented approach to planning and co-designing systems of care for patients, families and community members. By harnessing the power of community engagement, data, advanced analytics and new technologies, IBH is shaping the future of health care by working to foster healthier, more equitable communities.
Integrating Equity as a Key Component of Our Reporting Metrics
Inequities within the health care system are deeply entrenched, prompting health researchers and health systems to deploy new approaches to measure inequities with an aim to monitor and implement strategies to decrease disparities. At Trillium Health Partners (THP), the pandemic brought to light quantifiable gaps in our service provision, necessitating a concerted effort to understand where these gaps lie and uncover opportunities to intervene and reduce inequities.
THP leveraged the Relative Index of Inequality (RII) – a measure that can be calculated for many different services and tracked over time – to calculate differences in use across multiple services between those coming from high- and low-income neighbourhoods and reveal and act upon these disparities. The Ontario Breast Screening Program saw the widest discrepancies in utilization (i.e., service use that was 5.4 times higher among individuals residing in neighbourhoods with higher socioeconomic status in the 2021-2022 fiscal year); a stark realization given the importance of timely breast cancer screening in improving health outcomes. Findings from this project were presented at the Canadian Association for Health Services and Policy Research (CAHSPR) 2023 conference, and it grounds much of the other projects undertaken by the Population and Community Health team at IBH (described below).
The identification of substantial gaps through use of the RII facilitates targeted interventions and lays the groundwork for more equitable health care practices. As the first hospital to integrate RII into its operational strategies, THP sets a precedent for other health systems, signaling a shift towards proactive measures aimed at reducing disparities.
Through ongoing monitoring and strategic implementation of interventions informed by RII data, THP endeavors to create a health system that is safe and accessible for the diverse communities that we serve.
Understanding our Community and Emergency Department Tools

This year, IBH partnered with Mississauga Health (OHT) to launch the Understanding our Community Tool, a centralized resource designed to provide organizations within Mississauga Health and care providers across Mississauga with comprehensive statistics and insights into our community’s demographics and populations, segmented by neighbourhoods, to support service planning and decision-making with an aim to improve health outcomes. This tool is an important step in the work of Mississauga Health and THP to understand the diverse health needs of the communities that they serve.
This tool was co-designed alongside community partners, including IBH and Peel Public Health at the Region of Peel, patients, caregivers, Mississauga Health member organizations and Data Strategy Planning Table representatives. The tool provides insights into the sociodemographic characteristics of neighbourhoods across the Peel Region as well as specific insights into Emergency Department visits at THP among Older Adults and persons with a mental health and addictions visit.
The Understanding our Community tool outlines the demographics and health attributes of diverse communities across our Region and will serve to support future work related to service provision and system planning. With continuous updates and new data sources planned for in future iterations, this tool will provide the integrated data to facilitate informed decision-making and support efforts to improve health outcomes and reduce health disparities across the region.
Addressing Inequities in Cancer Screening
Significant disparities exist in cancer screening participation rates, which can also lead to uneven health outcomes, oftentimes faced by equity-deserving groups. Dr. Laura Rosella, Stephen Family Research Chair in Community Health and Scientist, alongside team members from IBH, THP’s Decision Support Team, and the Regional Cancer Program are leading work that explores current patterns and trends in cancer screening through a $1-million gift from the CIBC Foundation.
Led by a working group dedicated to reimagining cancer screening services in Peel, this project seeks to explore encouraging and discouraging factors to breast screening participation among groups in Peel that are typically underrepresented in screening, and to co-design, implement and evaluate solutions to recognized barriers to improve screening participation rates. These learnings will augment and enhance work that is currently underway with the RCP to co-design interventions with community members and health care provides to overcome barriers and rigorously evaluate the effectiveness of initiatives.
“Community members are the best people to identify what approaches will increase cancer screening participation for them,” says Dr. Rosella. “Co-design means we develop these new solutions in partnership with the community members who are experiencing barriers to cancer screening and the providers that deliver that care.”
Despite improved cancer survival, persistent disparities disproportionately affect certain populations. IBH is beginning with a focus on breast screening, aiming to expand the reach of programs to meet community needs, addressing awareness, access, equity and experience. The findings from this project can help benefit other cancer screening programs on a provincial, national and international scale and learnings will be scaled to inform other preventative services offered at THP.
Creating a New Kind of Health Care Through Innovative Thinking and Partnerships
Innovation is an important component of creating a new kind of health care for a healthier community. Advancements in virtual care, digital technologies and Artificial Intelligence (AI) are key to helping shape health care services and enhance the experience of patients and families and improve the health of the community by addressing the day-to-day challenges that Trillium Health Partners (THP) faces.
This year, IBH’s Innovation team in partnership with THP clinical program leadership tested Signal 1’s Clinical Stability Predictor in THP's Medicine Program and Emergency Department. The algorithm, developed at another Canadian hospital, was deployed in the Medicine Program through a six-month project supported by the AI Deployment and Evaluation (AIDE) Lab at IBH. Clinical Stability Predictor uses patient data from Epic, THP’s electronic medical record system, to predict patient status within 72 hours. This insight, paired with clinical expertise, helps care teams deliver the best patient care, enhance decision-making and improve efficiency and workflows, and is just one example of how IBH is innovating care delivery to benefit the local community and beyond.
Learn about some of the people and projects at the Institute for Better Health (IBH) that are creating better care through thinking differently, championing change and shaping a healthier tomorrow.

Improving Quality and Access Through the Virtual Hub
IBH has made significant strides in advancing its Virtual Hub operations, enriching digital care programs to improve access, reduce emergency department (ED) capacity and better serve our community. At the forefront of this progress is the Mississauga Health’ Seamless Care Optimizing the Patient Experience (SCOPE) program, which saw remarkable growth and impact in its first year. SCOPE is a virtual platform that connects primary care providers with a wide range of health care resources, including a general internist, home and community care coordinators and medical imaging, among others. Mississauga Health SCOPE is steadily positioning itself as the largest SCOPE program site in terms of onboarded physicians with 200 enlisted primary care providers since its inception in March 2023. Notably, Mississauga Health SCOPE facilitated 507 calls, resulting an impressive ED avoidance rate of 26 per cent.
The Long-Term Care (LTC) Virtual Care program has been instrumental in enhancing health care accessibility and diverting ED visits for LTC residents. With implementation across 13 LTC homes, the program has facilitated 485 consults since its launch in August 2022. The LTC Virtual Care program achieved an ED avoidance rate of 16 per cent, with an average turnaround time of 3.6 hours between request and specialist virtual visit.
The Community Paramedicine General Internal Medicine (GIM) support initiative continues to provide invaluable assistance to seniors facing complex health conditions. Community paramedics have initiated virtual GIM consults for over 65 community-dwelling seniors, resulting in 136 virtual visits by the end of March 2024.
With a total of 1,858 calls and virtual visits supported across these programs, IBH is committed to pioneering high-quality, accessible health care solutions to shape a healthier future.
Revolutionizing Clinical Trials with AI
The AI Deployment and Evaluation (AIDE) Lab at IBH is participating in a multi-centred initiative led by Altis Labs to develop Digital Twin models to revolutionize clinical trials for lung and colorectal cancer patients. The development of "digital twins," using patients' medical data will enable earlier and more accurate measurements of efficacy in trials while requiring fewer patients to be enrolled. The AIDE Lab, led by Dr. Benjamin Fine, Radiologist and Clinician Scientist, is curating CT imaging and electronic medical record data from our diverse THP population to support this important work.
Data Scientists at Altis Labs will be developing their models on THP data using our secure and governed AWS cloud platform. Hinging off the successful collaboration on this project, the AIDE lab will expand their work with Altis labs to include additional cancer disease sites with funding contributions provided by INOVAIT through the Government of Canada's Strategic Innovation Fund.
IBH Affiliate Scientist Receives 2023 Compassion and AI Grant from AMS Health Care
Dr. Andrew Feifer, Surgical Oncologist, Division of Urology, and Affiliate Scientist, Institute for Better Health (IBH), at Trillium Health Partners, was awarded one of the 2023 AMS Healthcare Compassion and AI grants for his work using machine learning approaches to predict tumour recurrence and progression to provide personalized and compassionate care for non-muscle invasive bladder cancer patients. “The opportunity to expand artificial intelligence utilization in urologic oncology is profound,” says Dr. Feifer. “It will allow us to better stratify the risk for patients to undergo therapy for invasive high-risk non-muscle bladder cancer, potentially alleviating the stress of treatment, better selecting patients for subsequent therapy and being able to care for patients more effectively regarding the nature of their illness.”
Advancing Patient-Centered Integrated Care Coordination
This year, Careteam Technologies, a cutting-edge Canadian digital health company with a focus on integrated care, acquired Care Connector, a unique patient-centred technology solution that was developed by the team at IBH to improve the integration and coordination of care planning.
Care Connector was developed internally at THP and co-designed with more than 2,400 health care providers by IBH to support and improve in-hospital team-based care and pre-discharge care planning and coordination.
Careteam Technologies and THP are partnering with the Mississauga Health Ontario Health Team, with a first deployment of the combined platform focused on enabling truly collaborative team-based care coordination of palliative care. Meeting the key priorities raised through co-design, the platform will empower patients, caregivers and families to have the ability to identify who is on their care team and invite them to the platform. Frontline providers will be connected to enable the seamless sharing of key information across partners and sectors to facilitate smooth transitions of care. The platform can be scaled to any clinical area across community and acute settings.
The development and acquisition of Care Connector highlight a commitment to patient-centred innovation and collaboration to transform the health care delivery and enhance patient and provider experience and coordination.
Trillium Health Partners
THP is committed to delivering high quality and exceptional patient experiences to our community of Mississauga and west Toronto.
Thanks to our Community and Donors
Working with our community and donors, Trillium Health Partners Foundation raises the critical funds needed to address the highest priority needs of Trillium Health Partners.











